Research and recent advances in epilepsy surgery
Can computer models help us improve the planning of epilepsy surgery?
The occurrence of seizures can pose a large burden on the quality of life of people suffering from epilepsy. When anti-epileptic medication is not enough to suppress the seizures, the clinical team often considers a resective surgery: the goal now is to remove the brain areas that are generating or generalizing the seizures. But the outcome is not as good as we would like: currently about 1 in every 3 patients who undergo epilepsy surgery continue to have seizures afterwards. In order to improve this outcome, so that patients have more changes of being seizure free after the resection, at Amsterdam UMC we are developing a computer model, personalized for each individual patient, that will help us identify the best resection for each case.
General Introduction
Basic concepts on the study of brain disorders
Computer Models
How do computer models of seizures work?
About us
Meet the researchers involved in this project and read about our current work
Model Demo
Visualize how seizures propagate in the model and test different resection strategies
Discussion Forum
In our discussion forum you can drop your questions or comments, and interact with the research team
Our pseudo-prospective study has now been published in the peer-reviewed journal Network Neuroscience: https://doi.org/10.1162/netn_a_00361
In the special issue of December 2023 we give an overview of the project, describing the most important methodological improvements and results of the scientific papers mentioned below. For details, see: https://epilepsiejournal.nl/article/view/18473/20216 (in Dutch). An English translation can be found here.
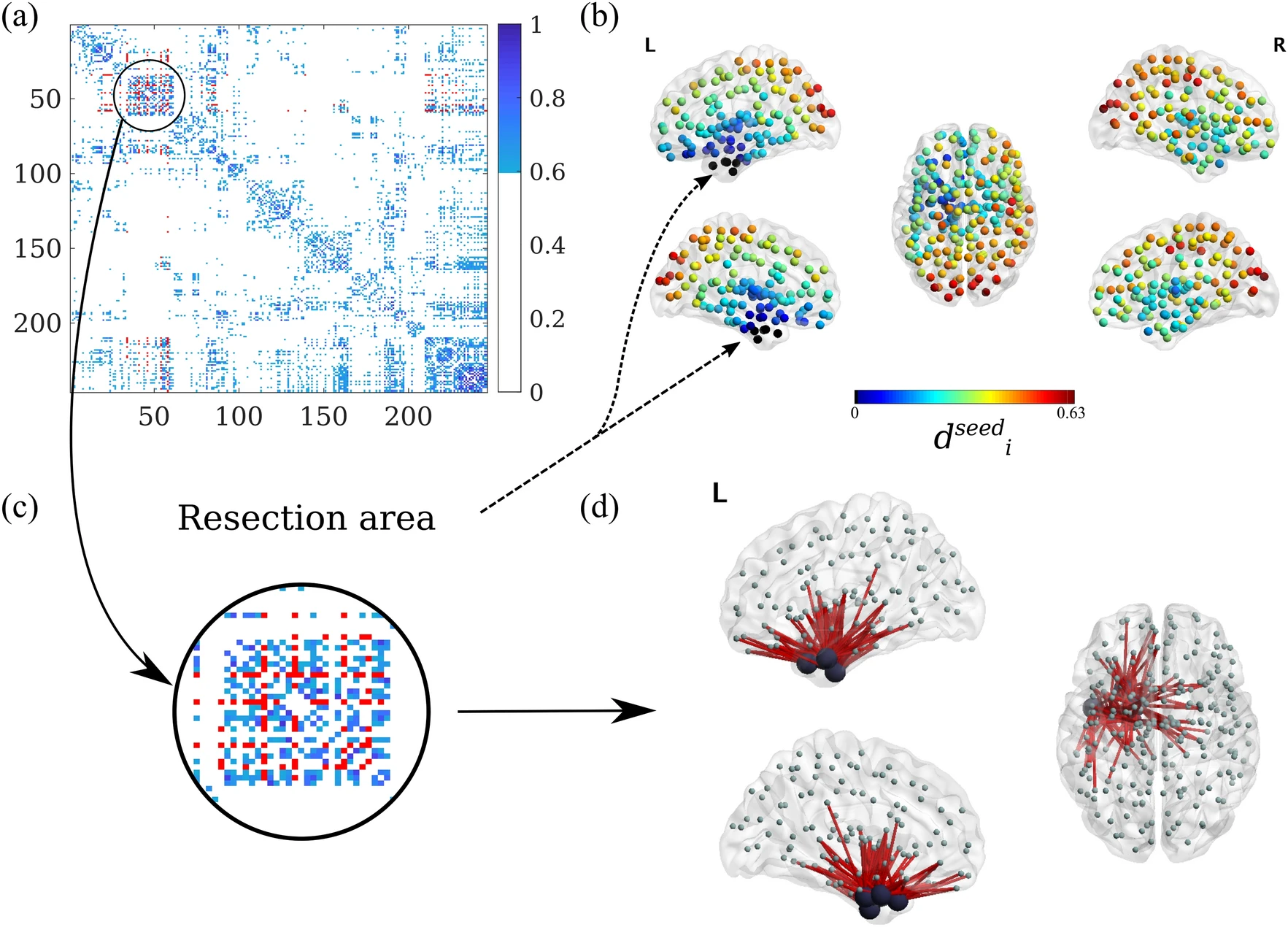
In a new article in Network Neuroscience, we build upon the previously published model for which the parameters were optimized by comparing the modelled patterns seizure propagation to the patterns observed in invasive EEG recordings.
Here, we further improved the model by adding a recovery mechanism (Susceptible-Infected-Recovered; SIR), which allows us to more easily determine the effect of virtual resections. Additionally, the start of the seizure is now determined by the model, allowing us to generate alternative hypotheses about the area where seizures begin. We were still able to successfully test the effect of virtual resections. The model is now ready to be tested in a (pseudo-)prospective study.